5 Proper Reasons To Lose Weight
Forget about looking good, forget about thin privilege, forget about fat privilege, forget about your personal rights and civic obligations, forget about your abs and your guns and your lats and whatever other laundry-list of nonsense is now used to describe your various bodyparts.
The thigh gap? Pure silliness. Of no consequence whatsoever.
Forget about your body image. Forget about Fat Wars, and shame, and size oppression, and the fact that you’re beautiful just the way you are (which is thin, or fat, or self-identifying as a mollusk, or whatever other wretchedness the internet has spawned this week). Put all this to one side. Leave it there.
Forget about all the normal scares — atherosclerosis, and arterial plaque, and cardiac arrest, and pulmonary hypertension, and stroke, and a laundry list of cancers, and diabetes, and metabolic syndrome. And while we’re at it, we can stop arguing about whether or not you specifically are at risk for any of them on the basis of some biomarker you just had measured:
“My glucose tolerance is good, I’m healthy and fat!”
“My triglycerides are low, I’m healthy and fat!”
“My cholesterol is excellent, I’m healthy and fat!”
Dear me. Let it go.
Forget most of all about Health At Every/Any Size. I’m not even sure what this is supposed to be any more. As far as I can tell, it’s the combination of three separate positions, used at the discretion of the arguer:
a) fat people have the right not to have rocks thrown at them in the street and to be treated with human dignity bc. they are people (very reasonable),
b) fat people should be exclusively supported in efforts to become more healthy, the first step of that health promotion is agreeing that social/emotional support is better than throwing rocks (mostly reasonable),
c) that obesity is a harmless lifestyle choice and/or accident of genetics and/or completely uncontrollable circumstance, and as a consequence health promotion should focus exclusively on topics other than weight loss, because obesity is of no more consequence than wearing a red sweater or driving a Nissan Sentra (in direct contradiction of available evidence, some of which I am about to address in great detail).
These wells are poisoned to me. You can’t move on the internet without people want to tell you how they feel about this. People feel very strongly, and a lot, and at random angles. These feelings make them upset and insane and hurtful, and they validate their feelings by battering others about the head and neck with them.
The intersection of body image, body fat and public health is a multiparous vortex of multiplying issues, and if history has shown us anything, it’s
- be scared when the white people turn up in boats, and
- no complex problem was ever solved by hooting on the Internet.
Let’s not feel. Or if that’s impossible, let’s corral those feels as much as possible so we can discuss just tissue.
Specifically, let’s discuss 5 areas of research in the health and medical sciences which provide good reasons not to be fat.
These reasons are alarmingly neglected in the public debate about obesity, nutrition, dietetics and exercise. Notice that I said public debate. They are not at all neglected in the RESEARCH into obesity, diet and exercise. They’re very well established, as we shall soon see, they just seem to be less well established in the public consciousness.
They are less alarming than arguments about whether or not you’re going to die.Or, for that matter, be diagnosed with something horrible. When we talk about public health outcomes, there’s a lot of focus on overall mortality from heart attack, stroke, cancer, etc. — things which don’t impair your health as much as take away your ability to have any. The reasons we’ll discuss are less … final than those, I suppose.
This doesn’t make them inconsequential, just less consequential than getting a horrible illness or dropping dead.
So, as might be expected, they broadly concern conditions which are mainlyquality of life issues. They certainly do bleed into the continuum of being alive vs. not being alive, but they are mainly concerned with how you live not how you stop living.
And they’re prevalent. One thing that has been (usually correctly) noted about associations between obesity and disease in studies of hundreds of thousands of people is that big increases in proportional disease risks are tempered by the fact that they are very minor risks in the first place. Let’s make up an example: if the risk of bladder cancer in normal weight people is 15 out of 10,000 and that goes up sharply by a WHOLE 60% (which sounds like a great deal!), that risk increases to 24 out of 10,000. It’s a minor overall risk which has become very slightly less minor.
These reasons are much more likely than the above, none of this 30% increase nonsense. Most of these issues are clear and present dangers — if you are fat, one or more of them are borderline guaranteed to directly affect you. We’re talking about big understandable increases in prevalence.
These are also very, very well evidenced reasons. You’ll see.
5. You should lose weight so you have knees
Obesity is a king-sized risk factor in the development of osteoarthritis. This is a degenerative joint disease characterised by the loss of cartilage and the destruction of bone joints.
It’s very common, because one of the primary risk factors is age, and the fact that everyone’s grandma has a twinge of it hides the degree to which it can be very unpleasant and debilitating.
Like most good chronic illnesses, it has a feedback mechanism. Your joints hurt, so you move less. Moving less means less joint loading and tissue turnover and muscle weakness (which means force doesn’t get cushioned correctly), which means the condition worsens… which means more pain. And onwards, we circle the drain.
We used to think obesity was just a matter of loading — more weight, more force over the knee joint, right? The classic paper on this is Hart and Spector (1993).
The age adjusted odds ratio (OR) [and 95% confidence interval (CI)] of radiographic OA at the knee comparing the high and low tertile of BMI was 6.17(3.26–11.71) and for bilateral knee radiographic OA was 17.99 (6.25–51.73). Comparing the middle and low tertile of BMI, the odds ratio for radiographic OA knee was 2.86 (1.44–5.68).
In English, this says the increase in properly diagnosed osteoarthritis of the knee between obese and normal people is more that 6-fold. In both knees, that rises to 18-fold.
(Other more recent estimates are lower. But the association has been replicated. A lot.)
What’s worse still — this isn’t just a matter of overloading joints. It’s a matter of adipose tissue (i.e. fat) being an active endocrine organ. In other words, the inflammatory environment created by excess fat seems to be provoking osteoarthritis over and above the effects of increased joint loading.
Adipose tissue, once considered a passive storage portal of energy, is now recognized as a highly metabolic endocrine organ with the capacity to secrete active agents including adipocytokines, such as leptin, resistin, and adiponectin. Over the past decade, interest in these adipocytokines has quickly become an area of intense study with respect to osteoarthritis based on evidence that they may play an important role in cartilage homeostasis and because of their emerging potential as therapeutic targets.
4. You should lose weight so you can sleep properly
Two words: sleep apnoea — “recurring episodes of upper airway collapse during sleep” a.k.a. something that is really bad for you.
There are a few straightforward mechanisms connecting body fat to the development of sleep apnoea. This paper isn’t recent, but as far as I’m aware there’s no evidence to invalidate any of the mechanisms it discusses:
(1) alterations in upper airway structure;
(2) alterations in upper airway function;
(3) alterations in the balance between ventilatory drive and load and
(4) obesity-induced hypoxemia
And the increase with obesity? Massive.
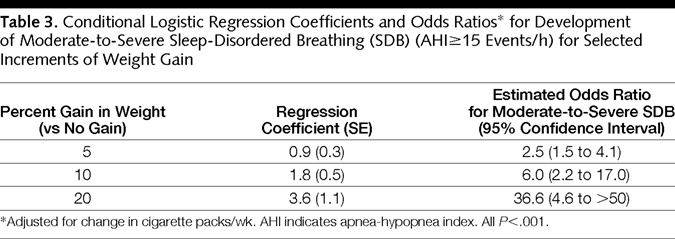
Table 3, Peppard et.al. (2000)
This is a prospective cohort study — they followed a large group of people over time to see the interrelationship between different bodily changes. The key numbers here are the odds ratios —2.5, 6, and 36.6 times more likely to develop clinically significant sleep-disordered breathing corresponding to a weight increase of 5%, 10% and 20% vs. none.
I told you the numbers would be big, didn’t I?
I can find an even scarier number for children though, albeit from a small study — 46% of obese children had sleep apnoea.
Typical incidence in general population children? Approximately 3%.
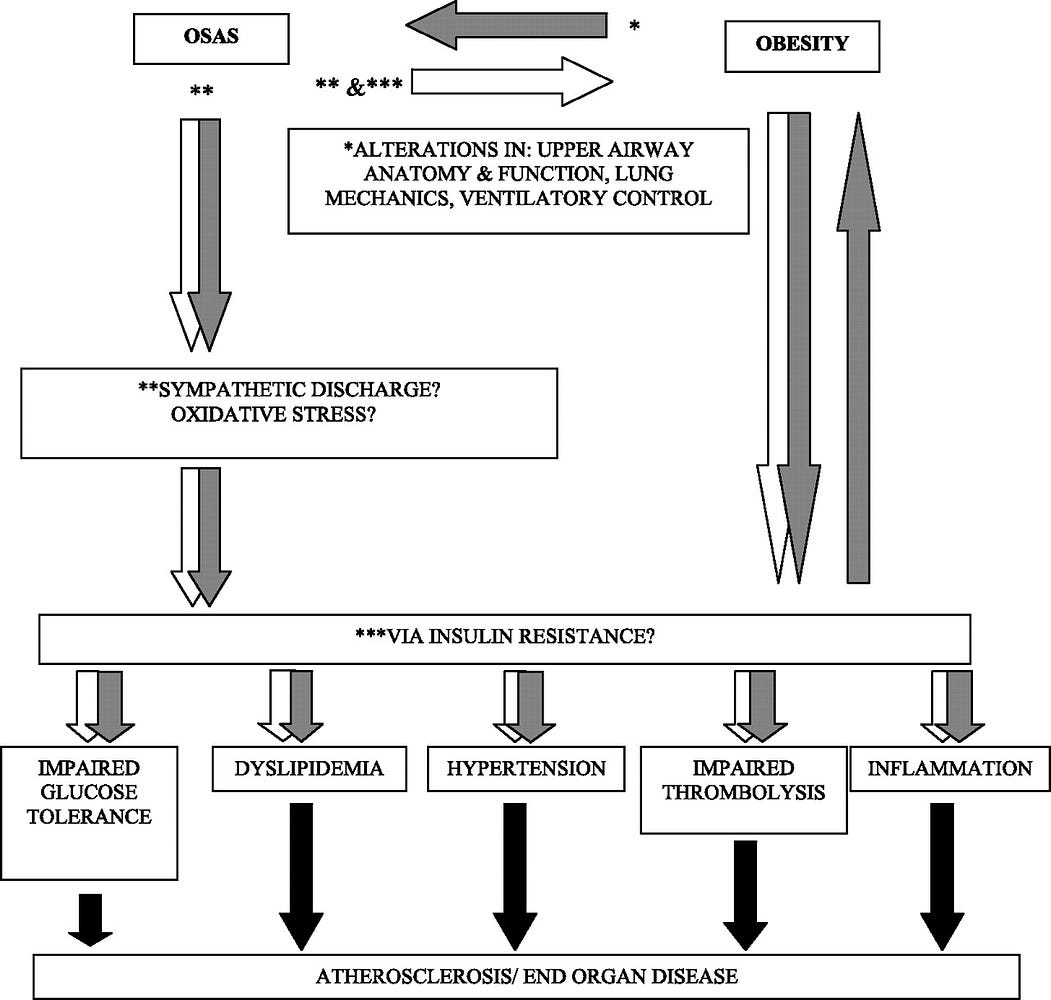
Oh, and as for why sleep apnoea is so bad, I’m going to let Arens and Mazumdar (2010) do the heavy lifting on that count, because it’s one of those intensely multifactorial situations which really is best described in a flow-chart rather than in text:
3. You should lose weight so you can taste properly
Wait, what? People who eat more food can’t taste as well?
Well, the best answer might be ‘sort of’. It would be more true to say that gaining significant weight seems to result in flavour perception which is fundamentally altered.
This is the issue here which is most seriously under-recognised, probably because we have to make the step from neuroscience research to human behaviour. Common messaging on diet/nutrition/exercise doesn’t come to that party.
(In fact, the literature in and around flavour perception and ‘reward deficiency’ rarely makes it out of the academic box at all… despite that, there’s a lot of fascinating research of the topic, which is also of immediate and direct relevance to weight management.)
Let’s start with the relatively straightforward human evidence.
First, oral sensitivity to fat (i.e. the strength and acuity of your ability to perceive ‘fattiness’) quite well predicts how much of it you eat:
The results from the present study support this proposition as individuals who were orally hypersensitive to C18 : 1 consumed less habitual fat and tended to consume less fat as a percentage of total energy intake. This observation is confirmatory to animal models, and strongly suggests that in human subjects, oral sensitivity to fats may be a determining factor in fat consumption.
So, fattiness is nice. What about traditionally unpleasant flavour profiles?
Facial expression results were consistent with our hypothesis, showing that bittertasting stimuli (grapefruit and chocolate) elicited significantly more intense disgust reactions and less neutral state reactions in the high BMI than in the low BMI condition.
(Interested readers can take on this, which is a literature review plus a more robust psychophysical exploration of the above.)
But for our purposes here, there seems to be an association between body fat and the sensitivity to both pleasant and unpleasant flavours. The next question is causality — is this something that you ‘learn’ if you gain weight, or is there a predisposition at work which means that certain types of ‘tasters’ are more likely to acquire different dietary habits?
In other words, we have something of a chicken/egg problem — which came first, the altered flavour preference or the extra kilos? And how modifiable are they?
Well, if the animal models can be believed:
- overfeeding obesity-prone mice results in changes in taste cell functionrelative to their litter-mates
- in rats, obesity-induced changes in fat/sugar reward are somewhat antagonised by subsequent weight loss
- rats given a gastric bypass (yes, that’s a real thing) appear to resume ‘normal’ liking/wanting behaviour
Now, those of you who have sharp eyes will have noticed that I haven’t framed this as a reason not to be fat. That’s because I’m out on a minor limb here. While the neurological evidence seems to quite robustly support the idea that normal taste processing is disordered in obesity, does thistechnically constitute a dysfunction?
From the simple perspective of wanting to maintain your normal interest and pleasure in food, I’d argue yes.
And how about prevalence? Who can we reasonably expect to be affected by altered taste perception? Well, I have no idea.
My suspicion, though, is everyone or almost everyone. Especially considering the most obesogenic foods just accidentally-on-purpose happen to pander directly to this dysfunction by having aggressively over-sweet, over-salty, over-fatty, etc. flavour profiles.
(For anyone interested in the practical applications of the above, which is called ‘hyperpalatability’, Mark Schatzker just wrote a book which will undoubtedly touch on this called The Dorito Effect. Which is a lot catchier than ‘hyperpalatability’. I haven’t read it yet, but I definitely will. And for an academic overview, Duffy (2007) is pretty great at tying all the loose ends together.)
2. You should lose weight to repair your immune system
I’m not an endocrinologist, so I found approaching this topic a bit more challenging than the others.
But as luck would have it there are two excellent and recent review papers on this — I shall now quote heavily from them, look clever by association and give my poor fingers a rest.
But how is obesity linked with the immune system?
The link seems to be adipose tissue itself. There are several connections indeed between adipose tissue and the immune system. For a start, macrophages and lymphocytes can be normally found in the non-adipose fraction of the tissue. Moreover, white adipocytes have been suggested to share embryonic origin with immune cells, while characterisation of adipose tissue-resident lymphocytes led to the notion that this tissue was an ancestral immune organ. …
Adipose tissue in general and adipocytes in particular secrete a great number of bioactive molecules of different nature, collectively termed adipokines, many of which have immuno-modulatory actions.
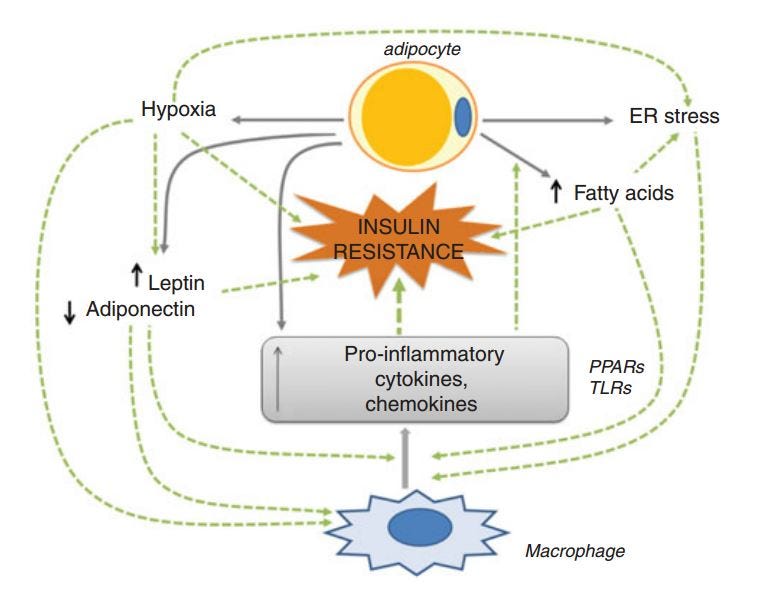
Figure 1:- the proposed link between adipocytes (fat cells) and macrophages (white blood cells on the ‘front line’ of your immune system)
“ …Increased BMI is associated with greater risk for several other bacterial infections including periodontal infections, Staphylococcus aureus nasal carriage and gastric infection by Helicobacter pylori…[and] significantly associated with herpes simplex virus 1 infection. …
It is well known that obesity is associated with a state of chronic, low-grade inflammation both in white adipose tissue and systemically. … It is possible that chronic exposure to pro-inflammatory cytokines may desensitise immune cells to inflammatory responses during an actual infection. …
Obesity clearly interferes with protection against infectious agents, and therefore increased research for a better understanding of the interactions between excess adipose-related metabolic abnormalities and immune cell activity is needed. Strong epidemiological evidence highlighting an association between obesity and infection is accumulating, and there are rodent models offering insight into potential mechanisms.”
I don’t think I can sum it up better than that.
And again, is this problem a) causal, and b) reversible?
Well, again, the evidence suggests yes.
As it says above, the link between excess bodyfat and the immune system is the fat itself — it isn’t just a passive storage unit, it’s an active endocrine organ. And in excess, a dysfunctional one.
1. You should lose weight so you live through surgery esp. childbirth
If I ever need surgery, I’m going to carve whatever spare bodyfat I’ve got off as soon as possible. In a sensible world, we’d be shouting this one from the rooftops.
- harder to intubate
- higher risk of incisional hernia post-laprascopy (i.e. popping open again)
- longer operation time
- higher risk of catheter site infection
- higher rate of serious postoperative complications
and on and on…
Seriously, pop any related search terms through PubMed and see the wonderful array of horrors you can find. Every anesthetist groans inside thinking about managing an obese patient.
And not only are post-operative outcomes worse, but put this together with the need for more operations in the first place. This isn’t just confined to things that only fat people get, like bariatric surgery. For instance, Caesarean birth rates are much higher… in the normal population it’s about 1 in 5, increasing to 1 in 2 in the morbidly obese.
And here’s a snippet from a review that I think is best quoted in full:
Narrative analysis of the 22 reviews included show gestational diabetes, pre-eclampsia, gestational hypertension, depression, instrumental and caesarean birth, and surgical site infection to be more likely to occur in pregnant women with obesity compared with women with a healthy weight. Maternal obesity is also linked to greater risk of preterm birth, large-for-gestational-age babies, foetal defects, congenital anomalies and perinatal death.
I think that’s about enough evidence for now.
Conclusion:
Let’s not pretend I’ve scoured the world looking for negative information, and I’ve cherry-picked the few precious bits available. Looking for academic sources for everything I wanted to say was extremely straightforward — I’ve just picked the most summarisable bits out of the towering mound of available evidence.
None of this is any secret, it just comes in a distant third in public discourse behind what we saw at the start:
- assorted boosting/scolding and body image issues: fat people are terrible/wonderful/shameful/naughty/victims/essentially self-destructive/essentially powerless/, and…
- public health discussion of life threatening and serious conditions: atherosclerosis, heart disease, stroke, hypertension, diabetes, metabolic syndrome, and other assorted nastiness.
This is something of a shame, because I seriously doubt that either side of the acerbic public debate over body size and morality is contributing anything towards solving the problem of keeping people alive and happy. And certainly, the collective recognition of the very serious health problems concomitant to the obesity epidemic doesn’t seem to affect behaviour a great deal.
I wonder if it’s time to talk about these more everyday things instead?
This is entirely apocryphal, but I have noticed a trend in the stories of people who lost a great deal of weight… they never say “I don’t think I’ll die at 55 now”, they focus squarely on their quality of life:
- “I can live in a walk-up apartment now”
- “I can run around with my kids”
- “I don’t get tired through the day”
- “Food tastes better. I can’t explain how…”
- “My random aches and pains stopped”
- “I couldn’t carry my two-year old without wheezing…”
- “I have so much more energy” (<- always suspect this is sleep related)
- “I bounce back from illness straightaway now”
And they always sound so satisfied. In the absence of some deeper psychological problem (which may well get WORSE, not better, with your waistline), I’ve heard or read a thousand stories of people who lost weight, and people always seem just a titchy bit better off.
Not by avoiding death, in the future. But by smoothing out the jagged edges of life, in the present.
Maybe this is the right messaging.
Maybe that’s what people managing their weight really need to know.
Maybe sore knees and pesky infections and bad sleep should see a little more attention, if we’re actually trying to help this problem along.
Food for thought.
Contact, stalk or send rough drafts of your Twilight fan fiction to James at his Facebook page.

![By Klearchos Kapoutsis (Flickr: The Puppy) [CC BY 2.0 (http://creativecommons.org/licenses/by/2.0)], via Wikimedia Commons The_Puppy](https://media.barefootfts.com/wp-content/uploads/2015/06/31120041/The_Puppy.jpg)